The rise of cashless claim settlements has transformed the healthcare experience for many in India. This convenient process eliminates the need for upfront payments at network hospitals, offering a smoother experience during medical emergencies. However, the system is not without its challenges.
Despite the advantages of cashless claims, a significant number of policyholders still resort to reimbursement claims. This article explores the reasons behind this trend, delving into issues like limited hospital networks, claim rejections due to time constraints, and misconceptions about reimbursement payouts. We’ll also examine the cashless claim process and the ongoing efforts to make “Cashless for All” a reality in India.
What’s on this page?
The Rise of Cashless Claim Settlements in India:
Cashless claim settlements have reshaped the landscape of health insurance in India, allowing policyholders to access treatment at network hospitals without upfront payments. Despite this convenience, many policyholders still find themselves filing reimbursement claims due to limited hospital access, claim rejections, and misconceptions about reimbursement payouts. Here, we explore why reimbursement claims remain common, how the cashless claim process works, and India’s journey toward making “Cashless for All” a reality.
Why Policyholders in India still Turn to Reimbursement Claims:
Despite the widespread availability of cashless facilities, several factors drive policyholders toward reimbursement claims:
- Limited Network Hospital Availability: The majority of network hospitals are concentrated in Tier 1 cities, with fewer options in Tier 2 and Tier 3 locations. While efforts to expand are ongoing, policyholders outside major cities often rely on reimbursement for treatment at non-network hospitals.
- Claim Rejections Due to Time Constraints: Cashless claim approvals are generally processed within four hours, per IRDAI guidelines. However, if the hospital, TPA, or insurer does not process the claim in time or if documents are incomplete, the cashless claim may be rejected, leading to reimbursement claims. For many, this is a critical factor, as cashless claims require a faster administrative response than reimbursement claims.
Misconceptions About Higher Reimbursement Payouts: Some policyholders believe they might receive a higher payout through reimbursement rather than cashless claims. In reality, cashless settlements are typically more cost-effective, as insurers negotiate lower rates with network hospitals. In reimbursement cases, hospitals may charge standard rates, which can lead to higher out-of-pocket expenses.
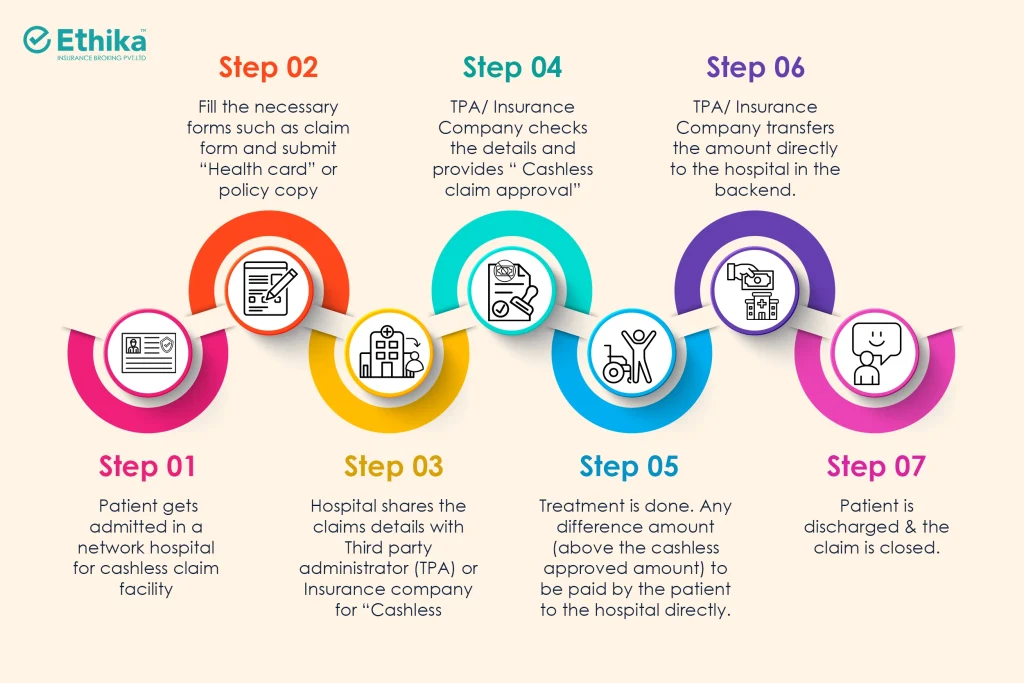
Cashless Claim Settlement Process: Step-by-Step Guide
Here’s a streamlined guide to the cashless claim settlement process:
Cashless for All : India’s Push Toward Inclusive Health Insurance:
The IRDAI has recently launched a Cashless for All initiative aimed at ensuring all hospitals, regardless of location or affiliation, provide cashless claim settlement for every policyholder. While this ambitious initiative is set to increase accessibility, it is still in the early stages of implementation. The goal is to bridge the gap between policyholders and healthcare providers, offering a consistent cashless experience across the country.
Embracing Cashless Health Insurance for All
The cashless claim settlement process has made healthcare more accessible and financially manageable for Indian policyholders. While challenges persist, such as network limitations and occasional claim rejections, initiatives like Cashless for All signal a promising future for inclusive and seamless healthcare financing. Policyholders are encouraged to familiarize themselves with the cashless process, use services of insurance brokers when needed, and leverage network hospitals to minimize out-of-pocket expenses.
FAQs
Can I Get Reimbursement at a Network Hospital?
Yes, if cashless approval is delayed or denied, you can opt for reimbursement even at a network hospital. However, be aware that rates for cashless claims are typically negotiated by insurers, so reimbursement rates may differ, potentially increasing costs.
How Long Does It Take to Approve a Cashless Claim?
IRDAI mandates that cashless claim approvals be processed within four hours. However, processing speed can depend on the hospital, TPA, and insurer. Delays or missing documentation can lead to rejections, which may require you to file a reimbursement claim.
Can I Use Cashless Without My Health Card or Policy Document?
Yes, a physical health card is not essential for cashless claims. In case of hospitalization, contact the designated person for your policy (or use the customer service helpline) to facilitate the process. Brokers can be instrumental in ensuring smooth communication and speeding up approvals.
Which is Better: Cashless or Reimbursement Claim Settlement?
Cashless claim settlement is generally preferable, as it eliminates the need for upfront payments and involves minimal administrative work for the policyholder. In reimbursement cases, however, you are responsible for filing, following up, and ensuring timely claim settlement.
What Should I Do if Cashless Approval is Delayed?
If approval is delayed, coordinate with the hospital, TPA, or insurer to expedite the process. Working with a broker can help, as brokers can effectively manage communication and reduce approval times.